Have you seen yourself or someone close to you dealing with memory, confusion, or personality changes? Dementia and Alzheimer’s disease are two terms that might create concern and provoke numerous questions, and that’s why Understanding Dementia and Alzheimer’s and their key differences is important. This comprehensive reference aims to provide you with information about various disorders, including symptoms, phases, management, and support services.
Explaining Alzheimer’s to Children
Instead of bombarding them with medical words, use simple analogies that they can connect to. For example, you could describe the brain as a particular computer that stores all our memories. Alzheimer’s disease might be like a small cloud in the computer, making it difficult to find and recall information.
Reassure the youngster that even if they forget things, the person with Alzheimer’s still loves them. They may just want additional assistance with daily duties such as remembering names or performing chores. Helping with these tiny tasks can be an excellent way for youngsters to express their love and support.
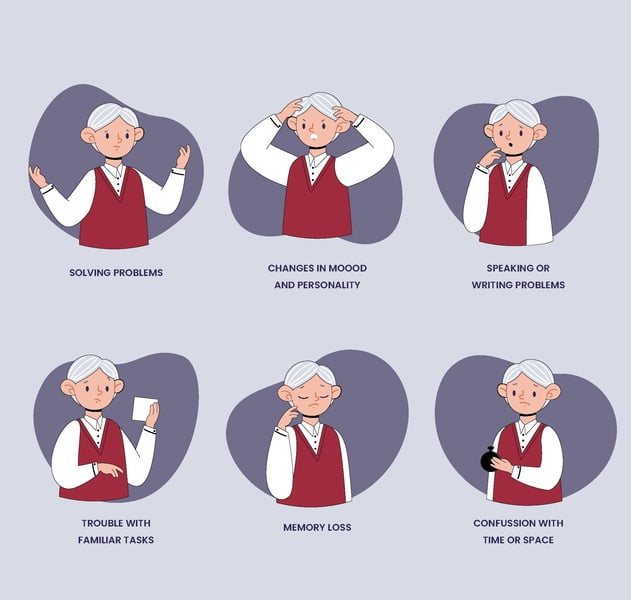
Symptoms of Alzheimer’s and Dementia
Dementia is a broad term describing a deterioration in cognitive functions that interferes with daily life. Alzheimer’s disease is the leading cause of dementia. Some common symptoms are:
- Memory loss refers to forgetting recent events, discussions, or the names of familiar people.
- Confusion is defined as difficulty understanding time, place, or what is going on around them.
- Changes in behaviour include increased anxiety, agitation, or retreat from social situations.
- Communication difficulties include difficulty finding the correct words or keeping up with conversations.
- Problems with judgement include making poor financial or personal safety judgements.
Understanding Short-Term Memory Loss
Our brains are continuously storing and retrieving information. Short-term memory functions as a brief holding area, helping us to recall information we recently learned or experienced. It functions like a notepad, allowing you to scribble down quick reminders. It is totally normal to forget what you just read or to misplace keys on sometimes.
However, short-term memory loss can be an early indicator of Alzheimer’s disease.
Identifying Risk Factors
While age is the most significant risk factor for Alzheimer’s, some things can enhance your vulnerability.
- Family history: Having a close family with Alzheimer’s disease raises your risk.
- Genetics: Certain genes are connected to an increased chance of acquiring Alzheimer’s.
- Lifestyle: Unhealthy behaviours such as smoking, lack of exercise, and a poor diet may all contribute.
- Medical conditions: High blood pressure, diabetes, and heart disease are all potential risk factors.
Addressing Misconceptions
There is a myth that persons with Alzheimer’s or dementia can “snap out of it.” These are progressive brain disorders. Understanding and assistance are essential for helping them live effectively with the disease.
Online Resources for Alzheimer’s
Here are some credible internet resources for information, support, and activism on Alzheimer’s disease:
- Alzheimer’s Association: Alzheimer’s Association
- National Institute on Aging: Alzheimer’s Disease Fact Sheet
- Dementia Society of America: Dementia Society of America
- Dementia Care Notes: Indian Website for Dementia
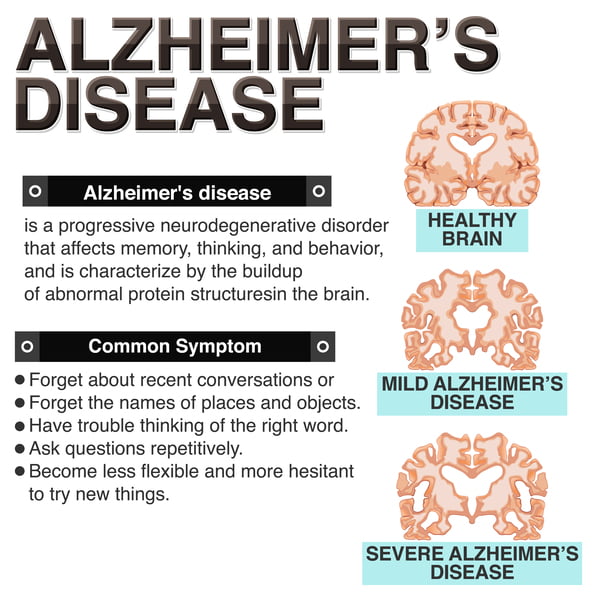
Explaining Alzheimer’s Disease
Alzheimer’s disease is a type of dementia that impairs memory, thinking, and behaviour. Symptoms eventually become severe enough to interfere with daily activities.
Imagine your thoughts as a bright, clear window. You can see things clearly and recall knowledge quickly. Alzheimer’s dementia is like a fog that slowly creeps in through that window. It makes it difficult to notice and remember details.
- Brain Cells Talk Less: In a healthy brain, brain cells constantly communicate with one another. In Alzheimer’s, protein clumps form and disrupt these talks.
- Memory Becomes Fuzzy: This fog makes it difficult to remember new things or recent experiences. You may forget where you left your keys or have difficulty recalling a recent conversation.
- Thinking becomes more difficult when the fog thickens. Daily tasks could feel more difficult.
Everyone’s fog moves at a different rate: Some people experience a gradual decline, while others may notice a more rapid change. The most important thing is to consult a doctor if you are concerned about yourself or a loved one. Early detection can aid in managing the fog and improving quality of life.
Early Signs and Stages
Alzheimer’s disease progresses gradually, with distinct stages marked by diverse symptoms.
Understanding the stages of Alzheimer’s disease
Alzheimer’s disease is a degenerative neurological disorder that impairs memory, thinking, and behaviour. It can be a complicated and overwhelming experience, both for the person living with it and their loved ones. Here’s a breakdown of the many stages, which provides a clearer understanding of how the disease could unfold:
Mild Cognitive Impairment (MCI): This is often the earliest and most subtle stage. You may discover that you or someone you care about is forgetful more often than normal. It could be that you’ve forgotten where you put your keys or are having trouble recalling a recent conversation. These memory lapses can be disconcerting, but it is crucial to note that MCI does not always indicate Alzheimer’s disease.
Early-Stage Alzheimer’s: As the condition advances, daily tasks may become increasingly difficult. Balancing finances, remembering appointments, and following complex instructions could become more difficult. You may find yourself depending on routines or asking assistance from loved ones to manage these activities. Don’t be afraid to ask for help; it shows strength and allows you to remain independent for longer.
Moderate Alzheimer’s: Memory loss becomes more noticeable during this stage. You may forget not only current events, but also recognisable people and long-held recollections. It may become challenging to navigate familiar environments or follow established routines. Personality changes, such as becoming more reclusive or easily frustrated, may also occur. Remember that these changes are not your fault, and there are ways to handle them.
Late-Stage Alzheimer’s: ndividuals suffering from Alzheimer’s frequently require entire assistance with daily routines such as bathing, dressing, and eating. Remembering loved ones or even recognising oneself in the mirror might be challenging. Physical decline may also occur, complicating the management of the disorder. If you are caring for someone at this stage, know that there are tools and support systems available to assist you get through this tough time.
It’s crucial to understand that Alzheimer’s disease develops differently for everyone. These stages provide a general overview, but the rate of change can vary greatly. Early detection and treatments are critical for improving the quality of life for those with Alzheimer’s disease.
Understanding Different Types
Dementia is an umbrella term, and Alzheimer’s is the most common type. Other types include:
- Vascular dementia is caused by a reduction in blood supply to the brain as a result of strokes or blood vessel diseases. The level of cognitive impairment varies according to the damaged brain regions and the severity of vascular injury.
- Individuals with Lewy body dementia, which is characterised by abnormal protein deposits that affect brain function, may experience a combination of mobility problems, hallucinations, and cognitive deterioration. The variable character of symptoms creates diagnostic challenges but highlights the importance of individualised treatments.
- Frontotemporal dementia affects the frontal and temporal lobes of the brain, causing significant behavioural alterations, personality shifts, and linguistic impairments. The variety of symptoms underlines the need for understanding and tackling the specific challenges presented by frontotemporal dementia.
Distinguishing Dementia from Alzheimer’s
Dementia is a general word for a deterioration in cognitive ability, but Alzheimer’s is a specific disease that causes dementia. Other disorders can induce dementia, although with different symptoms and progression patterns.
Life Expectancy for Dementia Patients
Life expectancy in dementia varies according to age, overall health, and kind of dementia. Early detection and treatment can help people live longer, more fulfilling lives.
Behavioural Triggers in Alzheimer’s Disease
People with Alzheimer’s disease may experience behavioural changes that can be challenging for both them and their carers. Some common behavioural triggers include:
- Stress and anxiety: Unfamiliar surroundings, changes in habit, or trouble communicating can all produce stress and anxiety, resulting in agitation or withdrawal.
- Confusion: Feeling confused or unable to comprehend what is going on can be frustrating, leading to tantrums or wandering.
- suffering: Alzheimer’s patients may be unable to convey their suffering vocally, which can lead to irritation and violence.
- Physical discomfort: Hunger, thirst, the need to use the restroom, or being too hot or cold can all cause behavioural changes.
- Sensory overload: Loud noises, bright lights, or excessive activity can be overpowering and cause uneasiness.
Duration of Stages
The seven phases of Alzheimer’s disease are a rough guideline, and the length varies greatly across people. It’s vital to remember that progress isn’t always linear. Here’s a quick overview:
- Stage 1 (early stage): Symptoms are moderate, with occasional memory lapses and trouble doing complex tasks. This stage can last several years.
- Stage 2 (Early to mid-stage): Memory loss becomes more evident, and confusion with familiar places or individuals may develop. This stage can span two to four years.
- Stage 3 (Mid-stage): Difficulties with daily activities such as dressing and bathing emerge. This stage can span two to four years.
- Stage 4 (Mid to Late Stage): Personality changes and sundowning (greater disorientation in the evening) may develop. This stage can last two to three years.
- Stage 5 (Late-stage): Individuals need substantial assistance with daily activities and may have difficulties talking. This stage can last one to three years.
- Stage 6 (Very late stage): Physical abilities deteriorate severely, requiring complete reliance on care. This stage can last one to two years.
- Stage 7 (End stage): Severe cognitive deterioration and physical limits develop.
It’s important to note that this is a general timeframe, and individual experiences can vary.
Sequence of Onset
Doctors may initially diagnose dementia before attempting to determine the precise cause, such as Alzheimer’s disease.
Progression to Alzheimer’s
Not all dementia progresses to Alzheimer’s. Different types of dementia, such as vascular dementia and Lewy body dementia, have distinct trajectories. Early detection and good care are critical components of improving quality of life. Being aware of various dementia forms is essential for developing personalised personal approaches that promote independence and general well-being.
End Signs of Dementia
As dementia progresses, the challenges become more difficult. People may lose their ability to speak, forget about loved ones, and struggle with everyday chores. They’re also more susceptible to illnesses, making the final phases both heartbreaking and risky. Despite these obstacles, compassionate care and support can provide comfort and dignity to persons in challenging situations.
Possibility of Recovery
There is currently no cure for dementia, although there are therapies that can help. These treatments act as tools, reducing symptoms and slowing the progression of the disease. The idea is to detect dementia early, so these methods will have the greatest impact. Regular check-ups with doctors are essential for early detection. Working with a healthcare team allows you to develop a strategy to manage the disease and help your loved one live as full a life as possible.
Stages of Dementia and Mortality
As dementia develops, the danger of death rises. Infections become a major worry. Hospice care provides comfort and support during this difficult time. Recognising the importance of hospice care in providing emotional support and pain treatment can provide relief to both patients and their families, assuring dignity and comfort in the later stages of life.
Golden Rules of Dementia Care
Here are three golden rules for dementia care:
- Empathy: Put yourself in the person’s shoes and try to understand their perspective.
- Communication: Use simple language, maintain eye contact, and be patient with responses.
- Safety: Ensure a safe environment free from hazards and provide supervision as needed.
Signs of Deterioration
If you notice a significant change in a loved one’s behaviour or cognitive abilities, it’s important to consult with a doctor. Signs of worsening dementia can include:
- Increased confusion and difficulty following conversations.
- Growing agitation or aggression.
- A decline in physical health or mobility.
- Loss of interest in previously enjoyed activities.
Early intervention can help adjust care plans and manage symptoms more effectively.
Remember, you are not alone on this journey. There are many resources available to help you and your loved one cope with dementia and Alzheimer’s disease.
A: Age is the strongest risk factor, but family history, genetics, unhealthy lifestyle habits, and uncontrolled medical conditions like high blood pressure and diabetes can also increase your risk.
A: Staying mentally and physically active, maintaining a healthy diet, managing blood pressure and cholesterol, and limiting alcohol and smoking are all positive steps you can take.
A: Increased forgetfulness, difficulty with familiar tasks, confusion, changes in mood or behavior, and problems with communication are all potential warning signs. Early detection is crucial.
A: While there’s no cure, medications can manage symptoms and potentially slow progression. They may improve memory, regulate mood, or promote sleep. Consult a doctor to determine the best treatment plan.
A: Support groups, respite care services, educational resources, and government assistance programs can all offer valuable help to caregivers.
A: There’s no guaranteed prevention, but a healthy lifestyle may help lower risk. Early diagnosis and intervention are key for managing the condition. While there’s no cure yet, research is exploring new treatment options and preventative strategies.
A: Social interaction stimulates the brain and may slow cognitive decline. Participating in social activities or spending time with loved ones can benefit your brain health.
A: The stages involve a gradual decline in cognitive abilities. Early stages may have mild forgetfulness, while later stages may require complete dependence on caregivers for daily activities.
A: Severe cognitive decline, loss of communication, difficulty controlling bodily functions, and increased vulnerability to infections are all common end signs.
A: Genetics can increase risk, but it’s not guaranteed. Having a close relative with dementia is a factor, but many others contribute to the development of the disease.
A: Yes, researchers are actively exploring new treatments. If interested in participating in a trial, consult your doctor to learn more about available options.
A: Research is focusing on new medications, brain imaging techniques for earlier diagnosis, and preventative strategies to potentially reduce the overall risk of developing dementia.