Pressure ulcers, often called bedsores, can develop when someone stays in the same position for too long. These sores are more than just uncomfortable – they can be painful, lead to severe infections, and significantly affect quality of life. This is especially true for people living with dementia, who are at higher risk due to mobility challenges and frailty.
But here’s the good news: with awareness and consistent care, pressure ulcers can often be prevented. Let’s explore how.
What Are Pressure Ulcers or Bedsores?
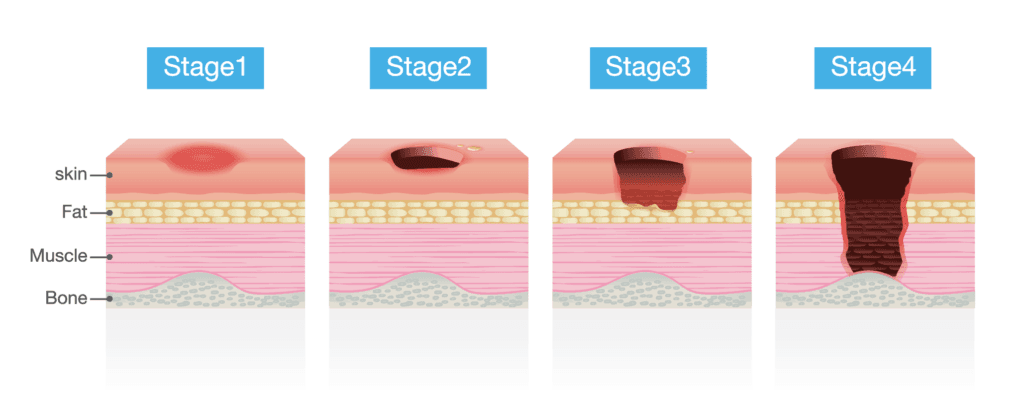
Imagine sitting on a hard bench for hours without moving. Eventually, you’d start to feel sore, and the skin under pressure might turn red. That’s the beginning of what can become a pressure ulcer. These ulcers happen when blood flow is cut off to an area, usually over bony parts like heels, hips, or the base of the spine. Without enough oxygen and nutrients, the skin and underlying tissue start to break down.
For those who are less mobile, especially older people or those with dementia, this risk increases significantly.
Why Are People with Dementia More at Risk of developing Bedsores?
- Mobility Issues: People with dementia may struggle to move or reposition themselves.
- Frailty: Thinner skin and less protective fat make ulcers more likely.
- Poor Nutrition: A lack of nutrients weakens the skin.
- Incontinence: Damp skin from leaks is more prone to damage.
- Communication Barriers: They may not be able to express discomfort.
Spotting the Warning Signs
Catching pressure ulcers early can make all the difference. Here’s what to look for:
- Red patches that don’t fade when pressed lightly.
- Hard, swollen, warm, or painful areas.
- On darker skin, watch for blue or purple patches instead.
Always check common problem areas like heels, ankles, hips, elbows, and the lower back when helping someone wash or dress.
How to Prevent Pressure Ulcers
1. Encourage Movement
- In Bed: Reposition every two hours. Use a timer or alarm if needed. Lifting aids can make this easier.
- In Chairs: Shift weight every 15–30 minutes. Standing and stretching helps, even for a few seconds.
2. Protect the Skin
- Ensure bedding is smooth and free from wrinkles.
- Opt for natural-fibre clothing (like cotton) to minimise irritation.
- Use pressure-relieving cushions or mattresses, available via community nurses or occupational therapists.
3. Improve Diet and Hydration
- A balanced diet with plenty of protein, fruits, and vegetables strengthens the skin. You will find this post useful 11 best foods to boost your brain and memory
- Encourage regular drinks to keep the skin hydrated and resilient.
4. Manage Incontinence
- Clean and dry the skin promptly after any leaks.
- Use barrier creams to protect delicate areas.
5. Avoid Friction
- When helping someone move, lift rather than drag them.
- Adjust their position in bed or chairs to prevent sliding, which can cause skin damage.
What If You Spot a Pressure Ulcer?
If you notice a sore, contact the GP or district nurse immediately. Early-stage ulcers often heal with simple changes like repositioning and using pressure-relieving aids. For more severe ulcers, professional care, including dressings and pain relief, may be needed.

Final Thought: Prevention Is Kindness
Pressure ulcers are more than a medical issue; they’re about comfort and dignity. By taking small, consistent steps – caregivers can prevent unnecessary pain and ensure their loved ones or patients feel cared for and valued.
Remember, it’s okay to seek help. Community nurses, occupational therapists, and organisations like the Alzheimer’s Society are there to support you. Together, we can make a difference in someone’s daily life.
Frequently Asked Questions
Bedsores, also known as pressure ulcers, are areas of damaged skin and tissue caused by prolonged pressure on the skin, often over bony areas like heels, hips, or the tailbone.
People with dementia are at higher risk due to limited mobility, frailty, poor nutrition, incontinence, and difficulty communicating discomfort.
Look for red, warm, or hard patches on the skin that don’t fade when pressed lightly. On darker skin, watch for blue or purple areas.
Bedsores often appear on pressure points like the heels, ankles, hips, lower back, elbows, and shoulder blades.
Encourage regular movement, use pressure-relieving cushions or mattresses, keep the skin clean and dry, and ensure they eat a balanced diet and stay hydrated.
Contact a GP or community nurse immediately. Early intervention can prevent the sore from worsening.
Mild bedsores (category 1) can heal with proper care, such as relieving pressure and keeping the area clean. More severe sores need medical attention.
Yes, bedsores can be extremely painful, especially if they are infected or left untreated. Pain relief, like paracetamol, is often recommended.
Special pressure-relieving mattresses, overlays, or cushions can help redistribute pressure and reduce the risk of sores. These can be provided by community nurses.
With consistent care and vigilance, most bedsores can be prevented. However, at the end of life, skin changes can make them unavoidable despite the best efforts.