Have you ever seen an older loved one struggle with memory, concentration, or problem-solving? These difficulties could be symptoms of dementia, a set of disorders that impair thinking and behaviour. However, dementia is classified into several forms, each with its own set of characteristics. Today, we’ll look at vascular dementia, which is characterised by reduced blood flow to the brain.
This article provides information about vascular dementia, including symptoms and causes, as well as treatment choices and management tactics. Understanding the disease will allow you to better navigate its progression and support people who are impacted. Early diagnosis and intervention are critical, so let us get started!
What is Vascular Dementia?
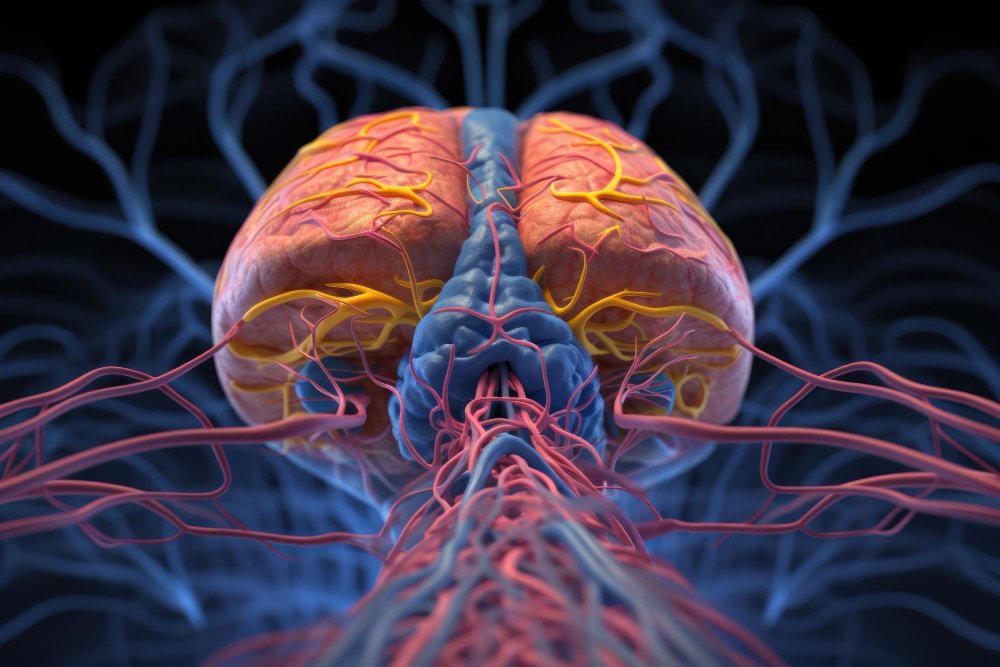
Vascular dementia refers to a group of cognitive and reasoning issues caused by abnormalities with blood flow in the brain. Unlike Alzheimer’s disease, the most prevalent type of dementia, vascular dementia is generally caused by strokes or other disorders that damage blood arteries.
Visualise the brain as a complicated city. Blood veins operate as highways, transporting oxygen and nutrients to various brain regions. When these highways become clogged or damaged, brain cells in those locations are deprived for necessary nutrients, resulting in malfunction and cell death. Depending on the location and intensity of the injury, several cognitive functions may be impaired.
What are the Symptoms of Vascular Dementia?
The symptoms of vascular dementia can vary depending on the areas of the brain affected by impaired blood flow. Here’s a breakdown of some common signs to watch out for:
- Cognitive:
- Difficulty with planning and organizing tasks
- Problems with attention and focus
- Slowed thinking and processing speed
- Challenges with problem-solving and decision-making
- Memory loss, often affecting recent events more than distant memories
- Physical:
- Difficulty walking or maintaining balance
- Urinary incontinence
- Speech problems, such as slurring or difficulty finding words
Progression of Symptoms:
Symptoms of vascular dementia frequently appear unexpectedly following a stroke or increase over time as a result of several smaller strokes. The pace of deterioration varies substantially from person to person.

Understanding Dementia: Types, Symptoms, and Treatments
Dementia is a general term encompassing a decline in cognitive abilities that interferes with daily life. It’s not a single disease, but rather a group of conditions with different underlying causes. Here’s a brief overview:
- Types of Dementia:
- Alzheimer’s disease: Characterized by protein buildup in the brain, leading to memory loss and progressive cognitive decline.
- Vascular dementia: Focuses on thinking problems caused by impaired blood flow to the brain.
- Lewy body dementia: Associated with abnormal protein deposits called Lewy bodies, impacting movement, thinking, and behavior.
- Frontotemporal dementia: Affects the frontal and temporal lobes of the brain, leading to personality changes, behavioral problems, and difficulty with language.
- Shared Symptoms: Memory loss, difficulty with thinking and reasoning, problems with communication, and changes in personality and behavior are common across various dementia types.
- General Treatment Approaches: There’s currently no cure for dementia, but treatments can help manage symptoms and improve quality of life. These include medications to improve memory, cognitive therapies to enhance problem-solving and daily living skills, and support groups for patients and caregivers.
What Type of Meds do Doctors Use to Treat Dementia?
While there’s no single medication to reverse dementia, some drugs can help manage symptoms and improve cognitive function, especially in Alzheimer’s disease. These include:
- Acetylcholinesterase inhibitors: Increase levels of a brain chemical called acetylcholine, which plays a role in memory and thinking.
- Memantine: Regulates glutamate activity, another brain chemical involved in learning and memory.
These medications can sometimes be used for vascular dementia as well, but their effectiveness may be less pronounced.
What is the Prognosis for Vascular Dementia?
The course of vascular dementia is variable. Some cases progress slowly, while others decline more rapidly. The prognosis can be influenced by several factors:
- Severity of blood vessel damage: The extent and location of brain damage determine the severity of symptoms and the rate of decline.
- Underlying health conditions: Managing conditions like high blood pressure, diabetes, and high cholesterol can help slow down progression.
- Lifestyle habits: A healthy lifestyle with regular exercise, a balanced diet, and good sleep hygiene can improve overall well-being and potentially slow down cognitive decline.
Is Vascular Dementia a Death Sentence?
Vascular dementia is a serious disorder, however, it does not always result in death. People with vascular dementia can live fulfilling lives for many years if they are managed and supported appropriately. Early diagnosis and therapy are critical for slowing the progression and preserving quality of life.
How Does Vascular Dementia Kill You?
In advanced stages, vascular dementia can lead to complications that increase the risk of mortality. Here’s how:
- Increased risk of falls and injuries: Difficulty with walking, balance, and coordination can lead to falls and fractures, which can be life-threatening, especially for older adults.
- Swallowing difficulties: Problems with swallowing can lead to aspiration pneumonia, a serious condition where food or fluids enter the lungs, causing infection.
- Malnutrition: As the disease progresses, individuals may struggle to eat independently, leading to malnutrition and dehydration.
- Increased susceptibility to infections: A weakened immune system can make people with vascular dementia more prone to infections, including pneumonia and urinary tract infections. These infections can become life-threatening in some cases.
Does High Blood Pressure Lead to Dementia?
High blood pressure (hypertension) is a major risk factor for vascular dementia. When blood pressure is uncontrolled for an extended period of time, it causes damage to blood vessels throughout the body, including those that supply the brain. This damage can cause restricted arteries, blood clots, and mini-strokes, all of which contribute to poor blood flow and ultimately cognitive impairment.
Here are some preventive measures to manage high blood pressure:
- Maintain a healthy weight: Excess weight puts extra strain on the heart and blood vessels.
- Eat a balanced diet: Limit salt intake and focus on fruits, vegetables, and whole grains.
- Exercise regularly: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Manage stress: Chronic stress can elevate blood pressure. Relaxation techniques like yoga or meditation can be beneficial.
- Medications: If lifestyle changes aren’t enough, your doctor may prescribe medication to control blood pressure.
Can You Recover from Vascular Dementia?
Unfortunately, there is no cure for vascular dementia, and brain cell loss is irreversible. However, early detection and therapy can greatly delay the disease’s course and enhance the quality of life.
Here’s why early intervention is crucial:
- Prevents further damage: Early treatment of underlying conditions like high blood pressure and diabetes can minimise further blood vessel damage and protect healthy brain tissue.
- Optimizes symptom management: Medications and therapies can be most effective when started early in the disease process.
- Improves quality of life: Early intervention allows individuals to maintain independence and participate in activities they enjoy for a longer period of time.
Which Treatment is Appropriate for Vascular Dementia?
The specific treatment plan for vascular dementia is tailored to the individual’s needs and the underlying cause. Here’s an overview of potential treatment approaches:
- Medications: As mentioned earlier, medications to manage blood pressure, cholesterol, and diabetes are crucial. In some cases, medications used for Alzheimer’s disease may be prescribed to improve memory and cognitive function.
- Rehabilitation therapies: Occupational therapy and speech therapy can help individuals with daily living activities and communication challenges.
- Cognitive rehabilitation: Techniques and strategies can be learned to improve memory, problem-solving, and other cognitive skills.
- Lifestyle modifications: Maintaining a healthy lifestyle with a balanced diet, regular exercise, and good sleep hygiene is essential for overall well-being and can potentially slow down cognitive decline.
What is the Behavior of a Person with Vascular Dementia?
People with vascular dementia may experience a variety of behavioural changes, including:
- Apathy and withdrawal: Loss of interest in previously enjoyed activities and social interactions.
- Irritability and aggression: Frustration with cognitive challenges can lead to outbursts of anger or agitation.
- Depression and anxiety: The awareness of cognitive decline and limitations can cause emotional distress.
- Personality changes: Individuals may become more impulsive, disinhibited, or exhibit unusual behaviors.
Tips for Caregivers:
- Remain calm and patient: People with dementia may have difficulty expressing themselves or understanding instructions. Be patient and communicate clearly using simple language.
- Validate their feelings: Acknowledge their frustration and emotions.
- Provide a safe and familiar environment: Minimize clutter and ensure the environment is easy to navigate.
- Establish routines: Create a regular daily schedule for meals, sleep, and activities to provide a sense of comfort and predictability.
- Seek support groups: Connecting with other caregivers can offer valuable advice and emotional support.
What are the Final Stages of Vascular Dementia?
As vascular dementia progresses to the later stages, symptoms become more severe, and individuals require increasing levels of care. Here’s what to expect:
- Intensified cognitive decline: Memory loss becomes more profound, and difficulty with communication and reasoning skills significantly impacts daily life.
- Increased dependence on others: Individuals may require assistance with all aspects of daily living, including dressing, bathing, and eating.
- Physical decline: Difficulty walking, maintaining balance, and potential incontinence become more common.
- Personality changes: Emotional outbursts, agitation, and apathy may become more pronounced.
Guidance for Caregivers:
- Focus on comfort and quality of life: In the later stages, the primary goal of care is to ensure comfort, manage pain, and maintain emotional well-being.
- Provide emotional support: People with dementia may experience fear, anxiety, and confusion. Be patient, reassuring, and offer comfort.
- Join a support group: Connecting with other caregivers can provide invaluable guidance and emotional support during this challenging time.
- Seek professional help: Don’t hesitate to seek assistance from home health aides, hospice care, or respite care services to manage the demands of caregiving.
What is the Latest Treatment for Vascular Dementia?
While there’s no cure for vascular dementia, ongoing research explores new treatment approaches. Here are some promising areas of exploration:
- Medications: New medications targeting specific aspects of vascular damage or neurotransmitter imbalances are being investigated.
- Lifestyle interventions: Studies explore the potential benefits of specific dietary patterns or exercise programs to slow down cognitive decline.
- Brain stimulation techniques: Techniques like transcranial magnetic stimulation (TMS) are being studied for their potential to improve cognitive function.

Who is at Risk for Vascular Dementia?
Several factors increase the risk of developing vascular dementia:
- Age: The risk of vascular dementia increases significantly with age.
- High blood pressure: Uncontrolled hypertension is a major risk factor.
- High cholesterol: Elevated cholesterol levels can contribute to blood vessel narrowing and hardening.
- Diabetes: Diabetes damages blood vessels throughout the body, including those in the brain.
- Heart disease: A history of heart disease or stroke increases the risk of vascular dementia.
- Smoking: Smoking damages blood vessels and increases the risk of vascular problems.
- Family history: Having a close relative with vascular dementia slightly increases your risk.
How to Slow Down Vascular Dementia?
While there’s no guaranteed way to prevent vascular dementia, certain lifestyle strategies can help reduce the risk and potentially slow down its progression:
- Manage underlying health conditions: Controlling high blood pressure, cholesterol, and diabetes is crucial.
- Maintain a healthy weight: Losing excess weight can improve overall health and cardiovascular function.
- Eat a heart-healthy diet: Focus on fruits, vegetables, whole grains, and lean protein sources. Limit saturated and unhealthy fats.
- Exercise regularly: Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
- Engage in mentally stimulating activities: Challenge your brain with puzzles, games, learning a new skill, or social interaction.
- Manage stress: Chronic stress can contribute to vascular problems. Relaxation techniques like yoga or meditation can be beneficial.
- Don’t smoke: Smoking significantly increases the risk of vascular disease.
Is Crying a Symptom of Vascular Dementia?
Crying and other emotional changes are common symptoms of vascular dementia. Here’s why:
- Brain damage: The areas of the brain responsible for emotional regulation can be affected by vascular dementia, leading to mood swings, tearfulness, or difficulty expressing emotions.
- Frustration and depression: The awareness of cognitive decline and limitations can cause frustration and depression, leading to tearfulness or emotional outbursts.
- Changes in communication: Individuals with dementia may struggle to express their needs and feelings verbally, and crying might be their only way to communicate distress.
What are the Signs that Vascular Dementia is Getting Worse?
Here are some indicators that vascular dementia may be progressing:
- Increased memory loss: Forgetting recent events more frequently, difficulty following conversations, or problems recognizing familiar faces.
- Greater difficulty with daily tasks: Struggling with tasks that were previously manageable, such as dressing, bathing, or preparing meals.
- Changes in personality and behavior: Increased agitation, apathy, or withdrawal from social interaction.
- Deterioration in communication skills: Difficulty expressing thoughts clearly, trouble finding words, or problems understanding conversations.
- More frequent falls or balance problems: Increased risk of falls due to impaired coordination and gait difficulties.
If you notice these signs, consult a doctor to assess the progression and adjust treatment
What are the Stages of Vascular Dementia?
While there isn’t a universally accepted staging system for vascular dementia, here’s a breakdown of the possible progression, categorized into early, moderate, and advanced stages:
Early Stage:
- Symptoms are often mild and might go unnoticed initially.
- Forgetfulness might involve misplacing objects or difficulty remembering recent events.
- Challenges with planning and organization may arise.
- Slowed thinking and processing speed might be subtle.
- Personality changes could be minimal.
Moderate Stage:
- Memory loss becomes more prominent, affecting both recent and distant memories.
- Difficulty with communication and following conversations increases.
- Confusion and disorientation become more frequent.
- Problems with judgment and decision-making become evident.
- Emotional outbursts, agitation, or apathy may be more pronounced.
- Dependence on others for some daily activities might be needed.
Advanced Stage:
- Severe memory loss significantly impacts daily life.
- Communication becomes very limited or even impossible.
- Disorientation and confusion are constant.
- Difficulty walking, maintaining balance, and incontinence are common.
- Personality changes become significant, with potential withdrawal or aggression.
- Individuals require complete assistance with all daily activities.
It’s important to remember:
- This is a general process, and each individual’s experience may differ significantly.
- The rate of decrease might be slow and progressive, or it can be quick, with step-by-step deteriorating following stroke.
- Early detection and intervention are critical for managing symptoms and improving quality of life at all stages.
Can You Live 20 Years with Vascular Dementia?
While there is no definite reason, surviving 20 years with vascular dementia is unusual. The usual life expectancy following diagnosis is between 5 and 10 years. However, there are various factors that can affect longevity:
- Severity of the disease: Individuals with mild forms diagnosed early can potentially live longer with proper management.
- Underlying health conditions: Effective management of co-existing conditions like heart disease or diabetes can improve overall health and potentially extend lifespan.
- Lifestyle choices: Maintaining a healthy lifestyle with a balanced diet, regular exercise, and good sleep hygiene can contribute to a longer and healthier life, even with dementia.
- Quality of care: Access to proper medical care, support services, and a safe and supportive environment significantly impact well-being and longevity.
Conclusion
Vascular dementia is a challenging condition, but with early detection and effective therapy, people can live productive lives for many years. Understanding the symptoms, risk factors, and treatment choices will help you better prepare for this journey. Remember, you are not alone. There are many tools and support groups available to help you and your loved ones manage with vascular dementia.
Frequently Asked Questions
Vascular dementia is primarily caused by reduced blood flow to the brain, which can be due to strokes, small vessel disease, or other conditions that damage blood vessels in the brain. These conditions can lead to cognitive decline when brain cells are deprived of oxygen and nutrients.
Early symptoms may include problems with planning, organizing, or making decisions, difficulties with attention, slowed thinking, and problems with memory or language. Mood changes and apathy can also be early signs.
Doctors diagnose vascular dementia based on medical history, cognitive tests, brain imaging (such as MRI or CT scans), and sometimes blood tests to rule out other conditions. The pattern of cognitive deficits and the presence of vascular brain changes help in making the diagnosis.
Managing vascular dementia involves maintaining a healthy lifestyle, including regular exercise to improve blood flow, a balanced diet low in saturated fats and high in fruits and vegetables, controlling blood pressure and cholesterol levels, and quitting smoking.
There are no medications specifically approved to treat vascular dementia itself. However, medications to control risk factors such as high blood pressure, diabetes, and high cholesterol may help slow its progression.
Untreated vascular dementia can lead to worsening cognitive decline, increased risk of strokes, and difficulties with daily activities. It can also contribute to other health complications due to decreased ability to manage self-care.
While vascular dementia cannot always be prevented, managing risk factors such as high blood pressure, diabetes, and high cholesterol can significantly reduce the risk. Treatment can also slow down its progression by improving blood flow to the brain and reducing the likelihood of further strokes.
High blood pressure is a significant risk factor for vascular dementia because it can damage blood vessels throughout the body, including those in the brain. Chronic hypertension contributes to small vessel disease and increases the risk of strokes, both of which can lead to vascular dementia over time. Managing blood pressure through lifestyle changes and medications is crucial in reducing this risk.